The pandemic has caused a large surge in mental illness, leaving many therapists busy and overwhelmed.
 People are not meant to spend their lives alone.
People are not meant to spend their lives alone.
As Aimee Amodio, a clinical social worker based in Portland says, “Humans are wired for connection.” So what happens when we are isolated, cut off from our family and friends and starved of social interaction?
In the midst of the COVID-19 pandemic, we are being forced to find out.
The tumult of the last two years has pushed a nation already struggling with mental illness to its limits. The COVID-19 pandemic has caused mental anguish all around the globe, with the World Health Authority reporting a 25% increase in anxiety and depression rates. In America, the demand for treatment is so high that the mental health industry is struggling to keep up, causing shortages of available therapists across the nation.
Mental health struggles are nothing new. According to the non-profit Mental Health America, in 2019, 18% of American adults reported experiencing mental illness and 12% of youth nationally reported experiencing a Major Depressive Event (MDE).
However, the COVID-19 pandemic and the turbulent nature of the past two years have worsened the problem. The combined impacts of prolonged isolation, economic uncertainty and worsening political division, have caused significant spikes in mental illness in Americans. The National Alliance on Mental Health (NAMI) found that around one in five people experienced a severe negative impact on their mental health because of the pandemic. For people already suffering with mental illness, that amount increased to almost half.
While the pandemic has stranded people from all backgrounds and age groups in the gloomy mists of mental illness, teenagers and youth have been hit the hardest.
“For high schoolers, having to be in school virtually for essentially two years (created) a lot of loss of socialization and being with friends, which creates a lot of sadness for people,” says Kayla Johnson, a therapist based in the Portland area.
A 2020 analysis by Mental Health America found a 9% increase in youth taking anxiety screenings compared to 2019. When comparing age groups, people aged 11–17 were most likely to score for moderate to severe symptoms of anxiety and depression.
As students returned to in-person schooling for the 2021-2022 school year, schools all across Oregon — including Roseway Heights Middle School and Reynolds Middle School — reported increases in fights, Title IX reports and other behavioral incidents. In November 2021, the behavioral issues at Reynolds forced the school to temporarily return to virtual learning.
Nearly a year and a half of online schooling and widespread isolation left many young people without the social skills necessary to resolve conflict. For many older kids and teenagers, the hardships of the pandemic have created deep feelings of helplessness and despair.
“I feel like all of these shots are being called and they’re just kind of subjected to them. And so I think it’s really stressful for youth,” says Andillon Del Pesco, the Youth Development Coordinator for Oregon Youthline.
Youthline is a mental-health crisis line for teenagers. It gives teenagers experiencing mental health issues the opportunity to speak anonymously with a teenage volunteer. Throughout the pandemic, the organization has witnessed its effect on teenagers firsthand.
“Our call volume in the year of 2013 was around 1200 contacts. And in 2020, we are at about 28,000 contacts,” says Del Pesco.
These significant increases in the amount of contacts are paralleled by similar surges in demand for treatment across the mental healthcare industry. “As the pandemic has gone on, more people have been seeking mental health support,” says Amodio, “They’ve noticed, like, ‘I’m handling stress differently, or I have more anxiety or I’m just depressed by all the news that’s coming out.’”
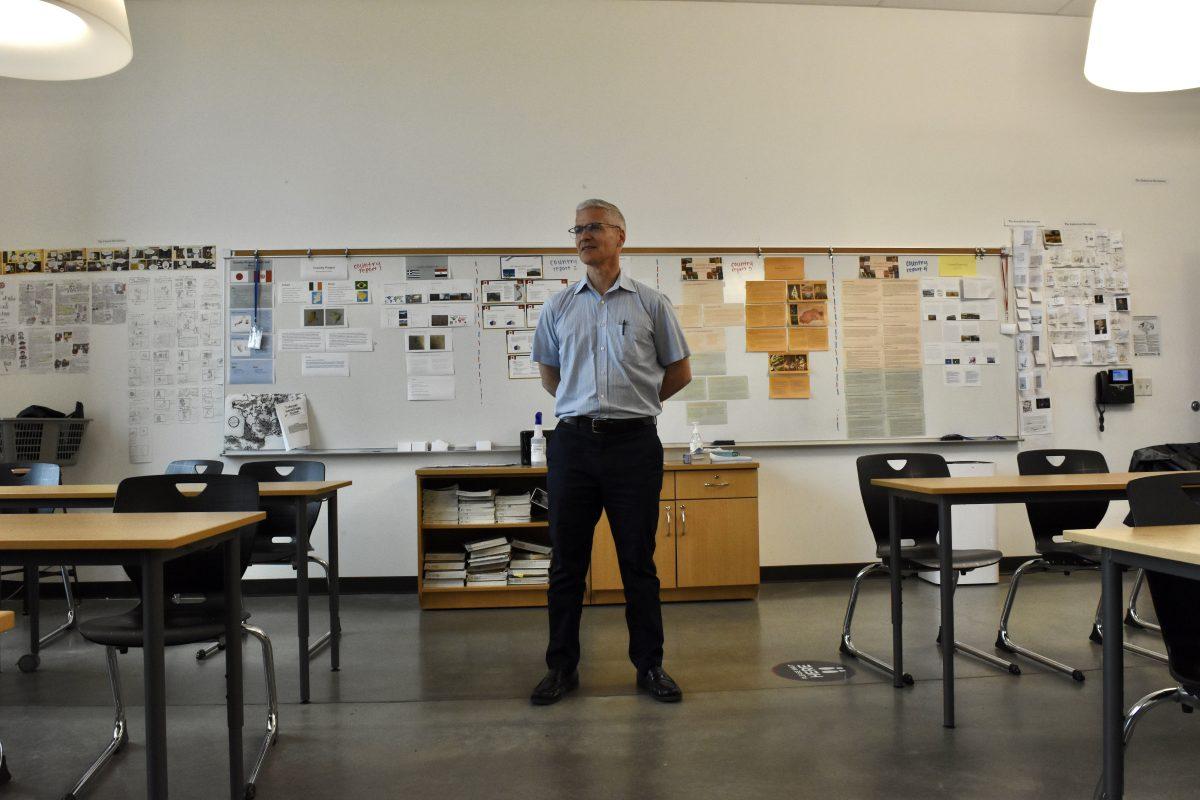
The high demand for treatment has left many therapists and mental health professionals overworked. Amodio has seen their number of clients increase by about a third, from around 15–20 people weekly pre-pandemic to about 26 now.
Some therapists are even busier. Claudia Fisher, a therapist in Washington state, provides mental-health treatment to those facing socioeconomic disadvantages. Before the pandemic, a high caseload for her would be considered 50 or more people. Her caseload right now is about double that.
“In the Vancouver-Portland area, the majority of clinics can’t accept new clients right now, because every therapist is at capacity,” says Johnson, “The whole system in general is really overwhelmed right now.”
High caseloads have left many therapists feeling stressed and burnt out. “I changed jobs about halfway through last year, sometime, kind of in the middle of one of the big surges of COVID,” says Johnson, “The burnout was so high that I couldn’t keep up anymore.”
Although the pandemic has brought challenges and stress to mental healthcare, it has also created some new opportunities. Like many services, therapists were forced to move their sessions online. Virtual healthcare, commonly known as telehealth, has enabled access to therapy for people who otherwise might find it difficult to get to an in-person appointment.
“A huge positive has been the opening of access to care, because instead of just seeing folks who live in my city, I now see folks all over Washington state and Oregon state,” Amodio says, “For the folks in rural areas, where they have to drive two hours to see a therapist or whatever, this is a huge plus for them.”
While telehealth is a great option for people who cannot get to an in-person appointment, therapists are worried. “I think the biggest concern that I’ve had during telehealth is I can’t really guarantee that my client has a fully confidential space,” Johnson says, “Because I don’t have any control over their environment, if they’re at home or if they’re in their car or wherever they might be.”
In addition to privacy concerns, telehealth may make it more difficult for therapists to connect with their patients. “One thing that’s really missing from telehealth is the ability to just kind of sit and share space with somebody and feel whatever they’re feeling … that’s been a downside,” says Amodio, adding, “There is evidence that telehealth is generally as effective as in-person mental health care, but that varies from person to person. And it even varies between, like, if you do a video call versus doing a phone call. So there’s even a difference with that level of feeling connected.”
However, this isn’t to say that quality therapy can’t happen in a virtual space; it just might take a little longer. “One of the top predictors of whether or not a person feels like therapy is helpful is the bond they have with their therapist,” Amodio says.
Amodio believes that persistence is key in receiving good therapy through telehealth. “If you stick with it and spend some time getting comfortable with each other, that’s when it works out to be generally as effective, but it can definitely feel like more of a struggle in that first month or two.”
The flexibility that telehealth provides has made it an appealing alternative for many therapists and their patients, and its use will likely continue long after the pandemic is over. “I think some form of telehealth is definitely here to stay … There are lots of therapists who are sticking with telehealth only. And then there’s many options in between, like hybrid. I’ll see some people in-person, some people virtually. I think it’s a good direction for mental health care to be heading in.”
Even as the pandemic wanes, the therapist shortage persists. Demand for treatment remains sky high, with therapists still struggling to keep up. It’s not hopeless, though — there are solutions to both the present shortage and the longer-term issues present within the mental healthcare system to ensure that all people have access to the mental health services they need.
Providing adequate support for therapists is the first step. There are many therapists, like Johnson, who have either changed jobs or quit working in the mental health industry entirely because of work-related stresses, further exacerbating the shortage. Making sure that therapists are able to take care of their own mental health is essential to ensure that they can continue helping others.
In the long-term, racial and ethnic disparities present in mental health care must also be addressed.“BIPOC individuals have less opportunity to access health care,” says Johnson, “And when you have less opportunity to access health care because your job doesn’t offer it, or you’re houseless or you don’t have a job … That’s gonna cause a whole other slew of trauma responses.”
Reducing these disparities would mean individuals could access treatment earlier and stop their mental health from getting worse, preventing any additional burdens on the system. It’s estimated that reducing health care disparities would have saved around 229 billion dollars nationwide between 2003–2006.
Properly addressing the problem of mental illness in America won’t just require changes within therapists’ offices. It will also require us to change the ways we interact with and support one another. “When we have not only belief in ourselves, but also people around us who believe in us and are able to give us a place to lean on when we need support,” says Amodio, “These are all things that increase your chances of feeling like you can bounce back from a traumatic event.”
Perhaps most importantly, we have to open up.
“Mental health kinda makes us want to isolate ourselves and withdraw,” Amodio says, “The actual healing thing is the opposite, to connect and be vulnerable and talk about what you’re experiencing.”